Healthy Youth Survey (HYS) 2023 Press Release
2023 Healthy Youth Survey results offer signs of hope and resiliency among Washington students
“The Healthy Youth Survey provides educators and policymakers with important insight into our students’ well-being,” said State Superintendent Chris Reykdal. “Our students are telling us that they are continuing to recover from the impacts of the pandemic––they are resilient, and hopeful, and they are getting access to the supports they need. While we still have work to do, the focused work of our educators, the support of our families and community members, and the resources provided by our Legislature are making a difference.”
The COVID-19 pandemic brought with it a large decrease, roughly 50%, in most youth substance use. While the long-term impacts are unknown, in 2023 we see that substance use has mostly remained stable, both in Washington and nationally, according to the 2023 HYS and Monitoring the Future surveys.
Visit www.AskHYS.net to access resources, explore the data dashboard, propose new or modified survey questions for 2025, learn about survey process, or how to advocate for your child’s school to participate in the next round.
For immediate release: March 13, 2024 (24-029)
Contact: DOH Communications
Full Press Release:
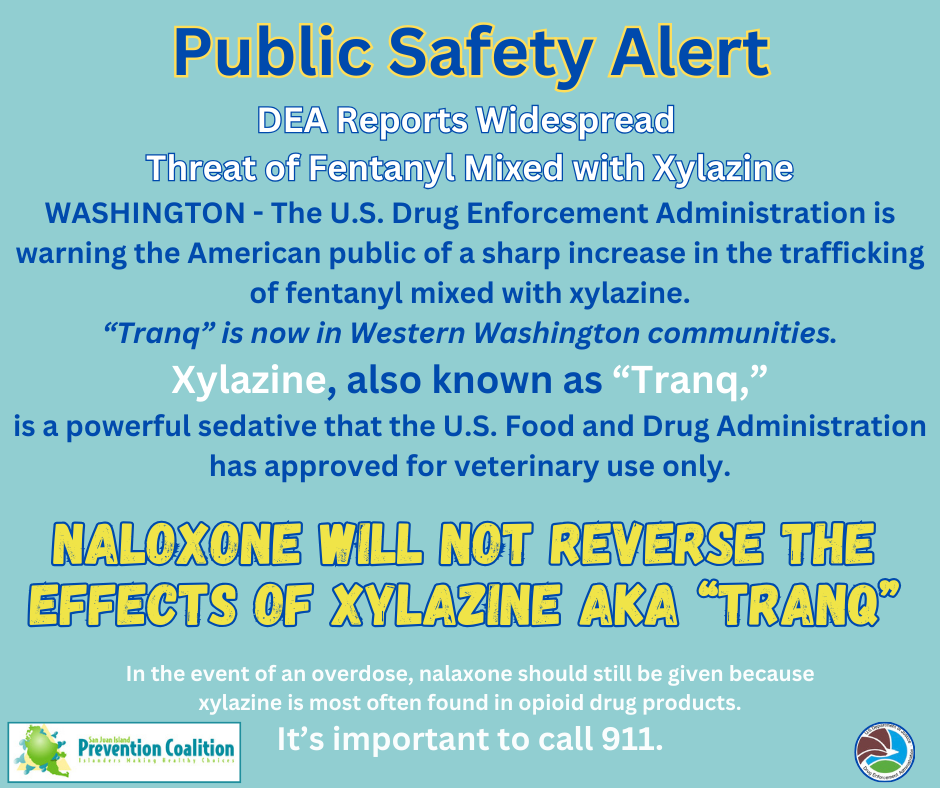
Public Safety Alert – “Tranq”
Middle School Peer 2 Peer Training is March 26, 2024
 Peer 2 Peer is a youth cannabis and tobacco prevention program created by United General staff to train high school and middle school students to become peer educators. After taking part in a fun, free training, peer educators are equipped with the knowledge, skills, and tools to teach younger peers and community members about health and prevention science, healthy coping skills for stress and anxiety, social norms, the effects of cannabis and tobacco, and more. Since its inception in the 2019-2020 school year, nearly 100 young people and their adult advisors from across the Northwest have been trained in the Peer 2 Peer curriculum, and we are thrilled to once again be offering these trainings in person.
Peer 2 Peer is a youth cannabis and tobacco prevention program created by United General staff to train high school and middle school students to become peer educators. After taking part in a fun, free training, peer educators are equipped with the knowledge, skills, and tools to teach younger peers and community members about health and prevention science, healthy coping skills for stress and anxiety, social norms, the effects of cannabis and tobacco, and more. Since its inception in the 2019-2020 school year, nearly 100 young people and their adult advisors from across the Northwest have been trained in the Peer 2 Peer curriculum, and we are thrilled to once again be offering these trainings in person.
Olivia Guelich, Luke Fincher and Rebecca – Peer 2 Peer Training Team.
Luke is our Youth Leader for our SJI Prevention Coalition’s youth prevention team, Rock Solid. While at WWU, Luke is able to commitment time to keep paying it forward to regional and local youth in Growing the Good!
About the upcoming training:
- This trainings will take place on March 26th from 9:00am – 2:30pm Anacortes.
- This training is provided at no cost to advisors or students and will include snacks and a lunch.
- Transportation is provided by SJIPC. (8am ferry to Anacortes required.)
- Students at FHMS can contact their school counselor, Claire or contact us at media@sjipc.org for more details.
Peer 2 Peer High School Training – Feb. 21, 2024
Happy New Year! Happy New You:)
We hope this new year brings good health, joy, connections, and a positive outlook to you and yours! Envision the positive!

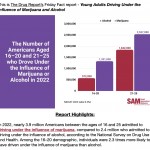
Data: Driving Under the Influence: Perceptions vs. Reality
Understanding the trends with young drivers and cannabis use behind the wheel. (See below) Perceptions of the dangers behind THC-impaired driving are misaligned with the reality. Correcting the misperceptions will help save lives.
Cannabis impairs many of the skills needed to drive safely.
Researchers found that cannabis use impairs: memory, learning, perception, motor coordination, attention (divided attention), motor performance (reaction time and tracking), cognitive performance, decision making and impulse control.
From Smart Approaches to Marijuana (SAM) is an alliance of organizations and individuals dedicated to a health-first approach to marijuana policy. We are professionals working in mental health and public health. We are bipartisan. We are medical doctors, lawmakers, treatment providers, preventionists, teachers, law enforcement officers and others who seek a middle road between incarceration and legalization. Our commonsense, third-way approach to marijuana policy is based on reputable science and sound principles of public health and safety.
Upcoming Peer 2 Peer Trainings Announced!
High School Training: February 21st 9:00am – 2:30pm
Middle School Training: March 26th 9:00am – 2:30pm
Registration for both the middle school and high school trainings will open after the holiday break on January 8th.
Training in Anacortes.
Contact us for more info, but here’s a little note from Olivia at United General.Peer 2 Peer is a cannabis and tobacco prevention program focused on empowering youth with the skills and confidence to teach their peers about health & prevention science, the effects of cannabis and tobacco, and healthy coping mechanisms for stress and anxiety.
The program consists of an all-day training for students where they will cover topics such as media literacy, presentation skills, have opportunities to practice delivering a prevention presentation for younger grades, and more!
After the training, students will be equipped with the knowledge and ability to create their own presentation about cannabis and tobacco prevention, and present that information to others within their communities.