ONLINE SURVEY ENGLISH
https://www.surveymonkey.com/r/SJSAJUEN2023

ONLINE SURVEY SPANISH
https://es.surveymonkey.com/r/SJSAJUSP2023
Please help us by completing our annual anonymous Community Survey for the San Juan Island Prevention Coalition. As you may know, this is part of our funding requirement by the State. We celebrate 20 Years of Growing the Good in our schools, community, and countywide collaborative efforts to support health.
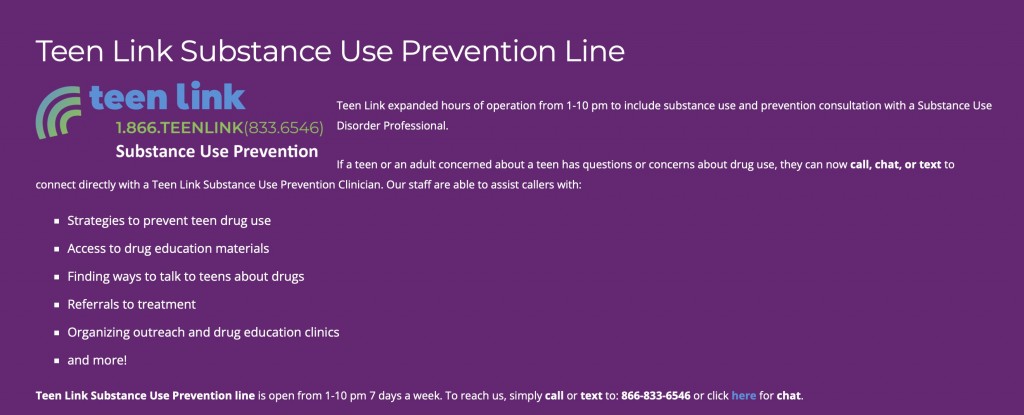
This survey provides the San Juan Island Prevention Coalition (SJIPC) with some local information about community perceptions. It looks at it as one point of data reference along with the Healthy Youth Survey, school intervention data that the Student Assistant Professional collects, and the program assessments for the programs that the SJIPC helps to fund: Community Based Mentoring and Strengthening Families provided by the SJI Family Resource Center, Second Step in the elementary school, LifeSkills Training in Grade 6 at FHMS, and the SAP (formerly the Prevention Intervention Specialist full-time position with now titled the Student Assistance Professional) that provides full-time prevention intervention support at the middle and high schools through support of the NWESD’s and the Coalition’s CPWI (Community Prevention and Wellness Initiative) partnership. Most importantly, CPWI has helped the SJIPC to support the growth of youth leadership prevention clubs, Rock Solid, HOTS, and HOT, Jr. The SJIPC has a robust social media presence that links to national, regional, and state public awareness campaigns.
Please help the SJIPC to gain continued support through the WA Health Care Authority’s Community Prevention and Wellness Initiative, which invests in our community by formalizing and supporting the coordination of community-based decision-making by completing this survey.
San Juan Island Prevention Coalition was founded in December 2003, began receiving federal Drug-Free Communities funding in 2004, and benefited from that support for ten years. SJIPC has sustained its work through CPWI funding, a mix of federal block grant funding (Substance Abuse Block Grant/SABG), and state Dedicated Marijuana Account (DMA) dollars. As a CPWI coalition, the SJIPC also have been able to receive federal Partnership for Success (PFS) supplemental funds that helped them to pilot the very successful Second Step program in grades K-5. Thank you!









 Congrats on another successful Peer 2 Peer Regional Training! United General’s new P2P Program Director, Olivia Geulich, along with their two Program Assistants and Peer Health Educators, Luke Fincher and Rebecca, inspired the next group of High School Peer Health Educators!
Congrats on another successful Peer 2 Peer Regional Training! United General’s new P2P Program Director, Olivia Geulich, along with their two Program Assistants and Peer Health Educators, Luke Fincher and Rebecca, inspired the next group of High School Peer Health Educators!