Please join the effort to raise awareness about overdoses.
An informational event will be held in Friday Harbor from 6:30 -8:30 p.m. at San Juan Island Public Library. Presenters will be Compass Health, San Juan County Sheriff’s Office, SAFE San Juans, and San Juan Island Emergency Medical Services.
Refreshments will be served. San Juan Island Prevention Coalition (SJIPC) has assisted Compass Health in organizing, marketing, and implementing the event because this is a very important issue that must be addressed collaboratively.
Members of the coalition are collaborating to help educate community members about the signs of overdose and the signs of depression, anxiety, and suicidal ideation that often lead to self-medicating and overdosing.
Please circulate the attached information within you circle of influence.
IOAD FlyerPoster.08312016.Final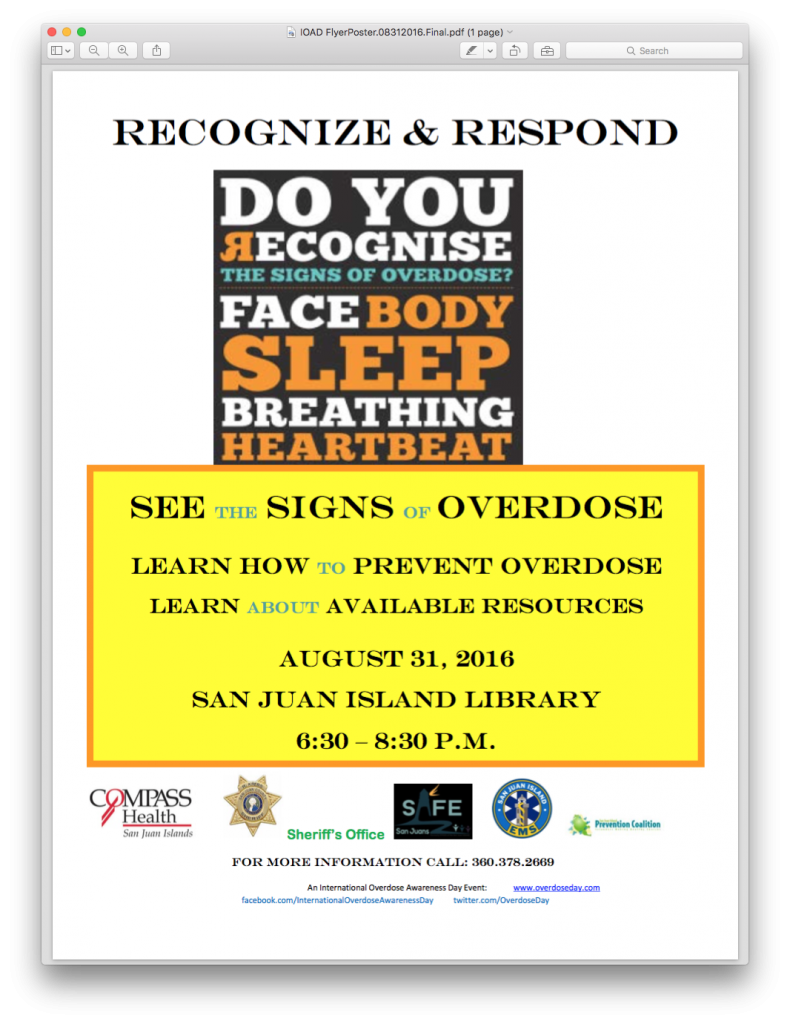
Recognize and Respond AGENDA
Learn How to Prevent OverDose
August 31, 2016
6:30 – 8:30
San Juan Island Public Library
- 6:30 to 6:45 Welcome and overview of purpose and outline of event, Barbara Starr, Mental Health Professional and Program Manager, Compass Health
- 6:45 to 7:10 Presentation by Shannon Reitan, Chemical Dependency Professional, Compass Health
- Prevalence of overdoses with various substances
- Importance of co-occurring disorders treatment
- Signs of overdose
- 6:10 to 7:30 Presentation by Ron Krebs, Sheriff, San Juan County Sheriff’s Office
- First responder actions
- Education for prevention and intervention
- Community collaboration efforts
- 7:30 to 7:50 Presentation by Kim Bryan, Director, SAFE San Juans
- Education for prevention and intervention
- Working with youth
- Community collaboration efforts
- 7:50 to 8:10 Presentation by Chief Jerry Martin, Chief and Lainey Volk, Education and Prevention Director, San Juan Island Emergency Medical Services (EMS)
- First responder actions
- Education for prevention and intervention
- Community collaboration efforts
- 8:10 to 8:30 Dialogue and Refreshments
An INTERNATIONAL OVERDOSE AWARENESS DAY Community Event www.overdoseday.com
What is an overdose?
An overdose means having too much of a drug (or combination of drugs) for your body to be able to cope with. There are a number of signs and symptoms that show someone has overdosed, and these differ with the type of drug used. All drugs can cause an overdose, including prescription medication prescribed by a doctor. It is important to know your correct dosage, what drugs definitely should not be mixed, and know to seek help if you feel you are not in control of your drug use.
Depressant overdose
Opioids, benzodiazepines & barbituates (medical Depressants), and alcohol all slow the central nervous system to produce a calming effect These substances are often prescribed to relieve pain, help you sleep, or in the case of alcohol, used recreationally when socialising. depressants, which means they slow the central nervous system, including breathing and heart rate. However, when taking in excessive amounts or in combination, they can depress normal functions such as breathing and heart rate until they eventually stop, resulting in death.
Opioids are narcotics which are either derived from opium (called opiates) or share a similar chemical structure but are manufactured without opium. Fentanyl, methadone, morphine and heroin are all opiates. Examples of opioids include oxycodone and hydromorphone.
Benzodiazepines are used medically to reduce anxiety, help people sleep and to relax the body. They include diazepam or Valium, oxazepam or Serepax , alprazolam or Xanax and a number of other drugs. Taken in high doses or in conjunction with alcohol they are responsible for many overdoses. Taking these kinds of drugs in higher than prescribed quantities can slow your breathing to dangerous levels or stop it altogether. Mixing these drugs can be extremely dangerous.
People’s tolerance to a drug can drop quickly and for a variety of reasons, such as having not used for a while (eg: having been in custody or having done detoxification/rehabilitation) or cutting down.
Signs of depressant drugoverdose (e.g. heroin, morphine, oxycodone, fentanyl, methadone) include:
- shallow breathing or not breathing at all
- snoring or gurgling sounds (this can mean that a person’s airway is partly blocked)
- blue lips or fingertips
- floppy arms and legs
- no response to stimulus
- disorientation
- unrousable (can’t be woken up) unconsciousness.
If you can’t get a response from someone, don’t assume they are asleep. Not all overdoses happen quickly and sometimes it can take hours for someone to die. Action taken in those hours could save a life. This is a medical emergency: call the ambulance immediately if you can’t rouse them.
Alcohol poisoning/overdose
Generally people do not automatically think of alcohol when they think of overdose, but alcohol is a depressant and it is all too possible to overdose on it. Acute alcohol poisoning, which is usually a result of binge drinking, is an example.
Our bodies can process about one unit of alcohol an hour. If you drink a lot quickly the amount of alcohol in your bloodstream (blood alcohol concentration, or BAC) may become dangerously high, which can stop your body from working properly. In extreme cases, alcohol poisoning could stop you breathing, stop your heart or cause you to choke on your own vomit.
Signs of alcohol intoxication to the point of overdose include:
- disorientation
- loss of coordination
- vomiting
- seizures
- irregular or slow breathing (less than eight breaths a minute)
- blue-tinged or pale skin
- low body temperature (hypothermia)
- stupor (being conscious but unresponsive)
- unconsciousness (passing out).
Stimulant overdose
It is possible to overdose on amphetamines such as speed and ice. Amphetamine overdose increases the risk of heart attack, stroke, seizure or drug-induced psychotic episodes.
Amphetamine overdoses look different from an opioid OD, and signs and symptoms include:
- chest pain
- disorientation/confusion
- severe headache
- seizures
- high temperature (overheating, but not sweating)
- difficulty breathing
- agitation and paranoia
- hallucinations
- unconsciousness.
Understanding tolerance and half-life
When a person uses a drug regularly they develop tolerance to it. This means they need to use more to get the same effect. Similarly, if a person hasn’t been using regularly – or if they’ve not been able to get drugs – their tolerance will drop. When people take their usual amount of drugs after a break from using, it could be too much for the body to cope with and lead to an overdose. This is why high-risk situations for drug overdose include post-release from prison, detoxification and rehabilitation. Someone on naltrexone can also be at risk if they use soon after stopping oral medication, or skipped a dose, or when the effects of a naltrexone implant have ceased.
“Half-life” refers to the time it takes for a drug to drop to half the strength of its original dose. Some drugs have a long half-life, for example some benzodiazepines. If a person has used yesterday, they may still have enough in their system today to overdose if they use more. Diazepam (Valium) has one of about 24 hours, so if you took 20mg yesterday you would still have approximately 10mg of diazepam active in your system today. If you were then to use heroin or morphine, you would have an increased risk of overdose as you would be using the opioids in addition to that 10mg of diazepam.
Mixing drugs
Taking more than one kind of drug at a time puts strain on the body and can increase both effect and the risk. For example, most heroin-related overdoses are caused when other depressant drugs are taken too. Alcohol and benzos like alprazolam (marketed as Xanax) and temazepam (Temaze) are depressants, and mixing them with drugs like heroin, oxycodone (Oxycontin®) or morphine (MS Contin®) greatly increases the risk of an overdose.
What to do if someone is overdosing
- stay with them and assure them everything will be okay
- if they appear unconscious, try to get a response from them (eg: call their name).
- If you can’t get a response put them in the recovery position and call an ambulance.
- Commence first-aid. Emergency operators can give CPR instructions.
- Keep an eye on them. People can go in and out of consciousness.
- If stimulants such as amphetamines are thought to be involved, a person may feel hot, anxious or agitated. Try to move them somewhere cooler and quieter. Or try to make the place quieter.
When to call an ambulance
People are often reluctant to call an ambulance for fear of police involvement or concern about the cost of a call-out. The police will only attend if there is a fatality or if their presence is requested, for example if the ambulance crew feel threatened. This is an issue worldwide.
In addition to unconsciousness, call for emergency help when someone is:
- having a seizure
- experiencing severe headache
- experiencing chest pain
- experiencing breathing difficulties
- extremely paranoid, agitated and/or confused.
It is not necessary for someone to have all of these signs or symptoms for them to be overdosing. Exhibiting only a few could still mean they are in trouble and need emergency help.
Don’t ignore gurgling and snoring
Snoring and gurgling can mean a person is having trouble breathing.
With substance use, especially substances that slow down the systems of the body (eg: benzodiazepines, opioids, GHB), snoring may indicate a serious and potentially life threatening obstruction of the airway.
The noise generated results from reduction in the size of the airway, and the result is a reduction in the volume of air that is able to move in and out of the lungs with each breath, and vibration of tissues around the airway as the comatose person struggles to move air in and out of the lungs. The larger the obstruction, the smaller the amount of air that gets in, and the greater the effort that is required to try and get air into the lungs. The obstruction occurs when the person is unable (due to their substance use) to move their head/neck/body to allow better air flow, and because collapse of the airway due to decreased muscle activity around the airway that normally keeps it open – this is because they are unconscious, not because they are sleeping.
In the setting of substance use, snoring is not something that should be seen as ‘normal’. Don’t let people ‘sleep it off’ if they are snoring – this may be a sign of significant and life threatening emergency – attempt to wake them immediately.
If they do wake then the snoring (airway obstruction) will resolve. If they do not wake, call emergency services and ask for an ambulance. Follow the instructions from the operator (you will probably be asked to roll the snoring person onto their side and open their mouth to maximise the flow of air).
Naloxone half-life
Naloxone (also known by one of the brands Narcan®) is the used by paramedics to revive people who have had an opiate or opioid drug overdose. Anyone who has been revived using naloxone needs to understand the danger of taking more drugs afterwards because they can overdose a second time. Naloxone can precipitate withdrawal symptoms which bring a powerful urge to take more drugs. Because naloxone has a half-life of 1-1.5 hours, considerably less than heroin and morphine, taking more opiates can bring on a second overdose. Drugs like methadone, and sustained-release opioids like OxyContin® and MS Contin®, provide the drug over 12 hours or more, so the effect of naloxone will wear off long before those drugs have exited your system.
Permanent brain damage and overdose
Hypoxic brain injury, which is caused by a lack of oxygen to the brain, is an under-reported consequence of heroin overdose. These brain injuries can cause coma, seizures and, in worst case scenarios, brain death. The long-term consequences of hypoxia depend on how long the brain is without adequate oxygen supply. Basically, the longer a person is not breathing, the more potential damage is being done to the brain. In many overdose cases such information is unknown. Health outcomes depend on the success of damage control measures, the area and extent of brain tissue deprived of oxygen and the speed with which oxygen was restored to the brain.
A brain injury can result in mild to severe impairment of:
- movement, balance and co-ordination
- senses such as hearing or vision
- spoken and written communication
- thinking, concentration and memory.
In severe cases, brain injuries from overdoses can leave people in a vegetative state.
Get the App
The Overdose Aware app aims to raise awareness amongst those who are experiencing drug use and their families, of how to recognize overdose signs and respond accordingly. More>>
Donate
International Overdose Awareness Day is committed to providing a platform to acknowledge the grief felt by families and friends who have lost a loved one to overdose. We aim to raise awareness that the tragedy of overdose death is preventable. Support our work today.
TRIBUTES
- My son, Travis, died of an overdose on July 28, 2015. He was only 23. He had been sober 3 months at the time of his death. I know that he fought so hard, and he was a beautiful soul trapped in the hell of addiction. I miss him every day and so wish I could tell him how much I love him and that I know he tried. Rest in peace sweet boy!